
Working in the hospital department, known as the OR, is not for the faint of heart. People here bring passion and commitment to their work.
“I love my job,” says Perioperative Nurse Educator Kelly E. Werthwein, MS, RN, CNOR. “I love the team respect. I love that everyone knows their job and does it well.”
Here, people work in teams.
They are methodical, vigilant, purposeful, and put the patient first. Because they work at a teaching hospital, they continually strive to learn.
“A teaching hospital means better patient care,” says Gary L. Freed, Jr., MD, who specializes in Plastic Surgery and Chronic Wound Healing. “It focuses you to stay contemporary while giving the best education you can get. It gets me excited to be here.”
“The culture of Dartmouth Health means everyone is learning and teaching and growing,” says Katrinia A. Rogers, BSN, RN, who is nurse manager of the Same Day Program where patients prepare for and recover after a procedure. “Patients have a lot of very invested professionals learning and caring for them.”
In that spirit of learning, collaboration, and delivering the best possible patient care, Freed, Werthwein, Rogers, and others have helped to provide this small window into how one outpatient surgery might unfold.
6:30 a.m. OR central hub
A steady stream of men and women in blue scrubs pass through automated, authorized-only entry doors before a central OR hub. A master scheduler turns on her screen to review this week's caseload, lit up in a big blue and green spreadsheet. The medical center has more than 20 surgery rooms operating daily, going by the shorthand names of vascular, plastics, ENT, eyes, ortho, general, ob-gyn/urology, cardio, neuro, and thoracic. Not seen are the surgical schedulers working in clinics and scheduling elective cases for patients across a five-week rotating block schedule. When a patient needs a more urgent procedure, centralized schedulers look at the next five days to determine when and where a case might be added to the schedule. The master scheduler at the central OR hub keeps track of these and answers surgeon requests to schedule patients that day.
6:30 a.m. Same Day Program
A man with an infected wound arrives. This hospital section has a total of 34 beds: 9 adult preoperative, 16 postoperative, 6 pediatric, and 5 regional nerve block beds for patients who have an orthopaedic procedure. Patients do not stay overnight but prepare for same-day procedures with an assessment that includes a review of medications, the start of an IV, signing consents, and meeting other pre-operative needs and requirements. The anesthesia and surgical team visit the patient, too.

Same Day Nurse Manager Rogers values, respects, and enjoys her colleagues, two of whom are pictured above with her. “We have the most cohesive team that I've ever worked for. Extremely supportive, very high functioning,” she says.
6:30 a.m. OR pre-surgery
A Perioperative Support Technician (PST) manages equipment, safety, and other environmental-related issues in this surgical room. The PST ensures all is sterilized, prepared, and properly equipped for today’s procedure, which will involve removing tissue and making sure the patient does not have an infected bone. Last night, Central Sterile Reprocessing sent up trays of sterilized instruments that a certified surgical technologist (CST) receives and oversees.
“I like to say we have significant patient impact and no patient contact. We do not get to see the really cool things our instruments do, but we have a high level of intelligence, learning and expertise,” says Sarah Tarleton, the Central Sterile Reprocessing Supervisor who works below on Level 2.

Meanwhile, upstairs in the OR room the circulating or scrub nurse and a nurse in training are already preparing and reviewing the upcoming case. A certified registered nurse anesthetist (CRNA) and a resident are present, too. Everyone is dressed in scrubs, masks, gloves and patterned or colored caps. Not visible are the compression socks beneath the scrubs. These people could be on their feet for 10 to 12 hours.
7:25 a.m. Patient transport from Same Day
The OR team pages Same Day to let them know the room is ready and the patient's chart is marked as ready, too. Staff prepare to transport the patient. If the patient is being monitored for cardiac issues, receiving medications, or is critically ill, additional medical providers join the transport team to provide support. A family member stays behind to monitor their loved one’s progress through a confidential number assigned to a screen in the Same Day waiting room.
7:30 a.m. OR surgery prep
The patient arrives at the plastics OR room. The circulating nurse identifies and talks reassuringly to the patient, explaining next steps and making certain the patient is comfortable and warm. An anesthetist enters, and the team moves the patient from the transport stretcher to the surgery bed. The patient is anesthetized and intubated. A Bear Hugger with a disposable warming blanket and reusable warming unit maintains the patient's core body temperature. The patient is positioned for surgery and covered in crisp, sterile drapes. The temperature of the room is cool. The team is intensely focused. A machine beeps, monitoring the patient’s heart, and each team member remains acutely attuned to the patient’s needs.
An educator watches through the OR room window. Her job as a preceptor is to train, mentor, and guide.

“Staff also train each other,” Werthwein later points out, stressing the collaboration and mutual support that exists within each perioperative surgical team and that is reinforced in the classroom pictured above.
8:00 a.m. Surgery begins
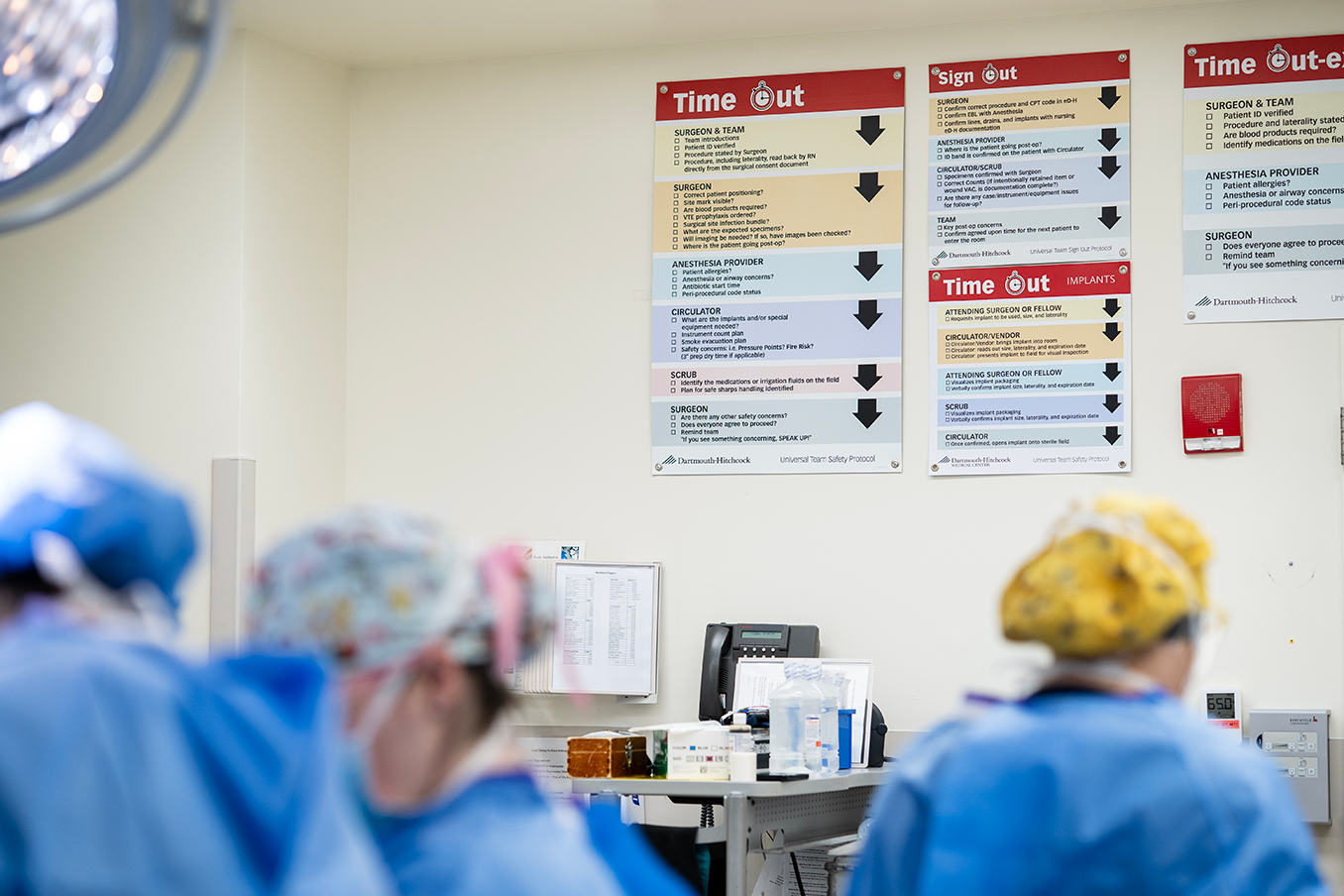
The surgeon for this morning’s procedure vigorously and methodically washes his hands, puts on gloves, peers through the surgery room window, enters the OR room, and warmly greets colleagues. The surgeon or circulating nurse calls the first Time Out, during which team members confirm the procedure, the correct side and position for surgery, and other details.
The surgeon makes the incision, exposing tissue, organs and bone beneath a bright spotlight. Vessels are cauterized, filling the room with a faint burning scent, as music plays quietly from the surgeon’s playlist. No one flinches at the smell, the blood, or the force needed to cut through tissue or scrape at bone.

The surgeon explains each step, as team members attend, listen, and provide needed instruments, the CST anticipating each request.
The circulating nurse manages the room. The resident stays at the surgeon’s side, and the nurse in training observes. Behind the curtain at the patient’s head is the CRNA, who watches, listens, and monitors vitals.
9:00 a.m. Surgery completed
The playlist is turned off. A second Time Out is called. Instruments are counted and everything is carefully tracked, including sponges discarded in a hanging pocketed drape that resembles a plastic shoe rack.
The incision is closed. The surgeon leaves to speak with the family member in the Same Day waiting room. The rest of the team stays with the patient. Dressings are put on, the body drape is removed, and the Bear Hugger is taken off. The anesthetist returns to the OR and joins the CRNA, who has remained steadfastly monitoring vital signs. Together, the team extubates and moves the patient off the surgical table before being transported to the Same Day recovery room on a bed embedded with a tray of sand to better distribute the patient’s weight and put less pressure on the wound.
9:30 a.m. After the surgery
Instruments return to Central Sterile Reprocessing and tissue samples are sent to the lab for analysis. Specimens too large to fit in a tube go to the master scheduler who dispatches them to the lab.
On one day, some 64 to 80 surgeries will occur across the OR. Same Day might have 160 patient encounters. Throughout the day, teamwork, vigilance, and a commitment to patient health and care prevail no matter the complexity of the procedure, and everyone strives to learn, paying close attention to what unfolds, including those observing through a small OR window like this one.