The aim of this retrospective analysis, of over 150,000 hours of medical/surgical unit continuous SpO2 and pulse rate data, was to investigate the impact of alarm configuration tactics in general care settings.
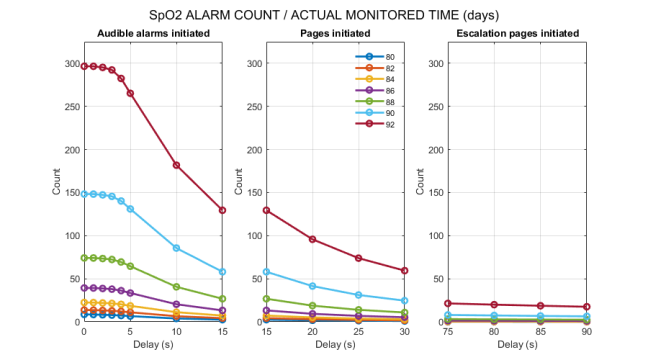
Application of an SpO2 threshold of 80% vs 88% produced an 88% reduction in alarms. Addition of a 15 second annunciation delay reduced alarms by an additional 71% with an SpO2 threshold of 80%. Pulse rate alarms were reduced by 93% moving from a pulse rate high threshold of 120–140 bpm, and 95% by lowering the pulse rate low threshold from 60 to 50 bpm. A 15 second annunciation delay at thresholds of 140 bpm and 50 bpm resulted in additional reductions of 80% and 81%, respectively.
Combined alarm frequency across all parameters for every 24 hours of actual monitored time yielded a rate of 4.2 alarms for the surveillance configuration, 83.0 alarms for critical care monitoring, and 320.6 alarms for condition monitoring. Total exposure time for an individual nurse during a single shift ranged from 3.6 min with surveillance monitoring, to 1.2 hours for critical care monitoring, and 5.3 hours for condition monitoring.
Previous studies have shown that continuous monitoring can eliminate unwitnessed/unmonitored arrests associated with significant increased mortality in the general care setting. This study adds to the literature by showing that the “alarm problem” associated with surveillance monitoring systems is manageable using alarm settings that signify severely abnormal physiology to alert responsible clinicians of urgent situations.
S. P. McGrath, I. M. Perreard, K. M. McGovern, and G. T. Blike, “Understanding the ‘alarm problem’ associated with continuous physiologic monitoring of general care patients,” Resuscitation Plus, vol. 11, p. 100295, Sep. 2022, doi: 10.1016/j.resplu.2022.100295.